Understanding how different cell types respond to exercise could be key step toward exercise as medicine
By Katharine Miller
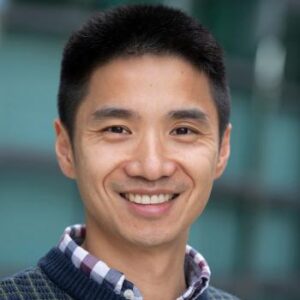
Researchers have long been fascinated by the possibility that exercise causes various cells in our body to produce molecules that benefit human health, says Jonathan Long, assistant professor of pathology at Stanford University.
If these molecules, which are sometimes called exercise factors or exerkines, can be identified and harnessed for pharmacological purposes, the theory goes, they might reduce the incidence of certain health problems such as obesity, heart disease and diabetes, as well as improve athletic performance.
But that goal has remained elusive largely because it has been impossible to isolate exerkines from the blood, Long says. “If you analyze whole blood, you can only see the most abundant substances in it and everything else is invisible.”
Now, however, Long and his team have developed a novel technique that can look much deeper into the blood to identify cell-secreted molecules. The technique also reveals which cell types produce which molecules – key information for better understanding the role exercise plays in improving health.
And Long’s novel method has now yielded a Cell Metabolism paper demonstrating the myriad ways that exercise changes the secretion of proteins by 21 different cell types in mice. The work, which was supported in part by a grant from the Wu Tsai Human Performance Alliance, also yielded a few surprises.
First, the sheer number of proteins whose presence in the blood changed in response to exercise was larger than anticipated. Indeed, the team found nearly 200 different exercise factors whose expression was either up- or down-regulated by the 21 cell types. “This means that the effects of physical activity are very widespread across many tissues and organ systems,” Long says. “We’re only just starting to understand that complexity.”
Second, the cells that were most responsive to exercise were a poorly understood type of cell that is named for a particular protein receptor (Pdgfra) and is found in many different tissues and organs. In fact, the usual suspects such as muscle, bone, and liver cells, only had moderate responses by comparison, Long says. “If we really want to understand the exercise response, we can’t just focus on muscle and bone and the other tissues we associate with exercise,” he says. “We have to look much more widely.”
The team was additionally surprised to find that liver cells – and only liver cells – secrete several members of the carboxylesterase family of proteins following exercise. Researchers have previously focused on these proteins’ functions within a cell and shown they were beneficial to metabolic health, but they hadn’t observed a possible role in the bloodstream.

To better understand their role, Long’s team engineered mice that secreted heightened levels of carboxylesterase proteins from the liver without exercise. And, it turned out, these mice resisted weight gain on a high fat diet and exhibited improved endurance on a treadmill. “These carboxylesterases are sufficient to confer some of the metabolic benefits of exercise without the animals themselves exercising,” Long says.
The study raises many questions for follow up. What role do Pdgfra cells play in different tissues and why are these cells responding to exercise? Just as the carboxylesterases show a metabolic benefit, might other exerkines have important anti-inflammatory effects or other beneficial effects on bones, the heart, the immune system, and the brain? In humans, do the levels of blood-carried carboxylesterases change in response to exercise as they do in mice?
From a basic science point of view, Long hopes this work will improve our understanding of cell-to-cell communication. But from a 30,000-foot view, there’s another reason to do these types of laborious research studies: The unrealized promise of “exercise as medicine.”
We know exercise has a therapeutic effect in many of the most chronic and debilitating diseases, but exercise is not like a medicine yet, Long says. That’s because most medicines consist of well-defined molecules with well-defined mechanisms of action, pharmacokinetics and pharmacodynamics, and adverse effects. By contrast, none of those things are well-defined for exercise, he says. “In the long term we want to understand the molecules and cells associated with exercise at high resolution so that exercise as medicine can become a reality.”
This work was done in collaboration with the Wu Tsai Human Performance Alliance’s Molecular Athlete program. Co-authors include Wei Wei, Nicholas M. Riley, Xuchao Lyu, Xiaotao Shen, Jing Guo, Steffen H. Raun, Meng Zhao, Maria Dolores Moya-Garzon, Himanish Basu, Alan Sheng-Hwa Tung, Veronica L. Li, Wentao Huang, Amanda L. Wiggenhorn, Katrin J. Svensson, Michael P. Snyder, Carolyn R. Bertozzi
Running image credit: Rawpixel.com/Adobe Images
Media Coverage: New Scientist, Neuroscience News
Latest News
February 9, 2026
Announcing the 2026 Agility Project awardees

January 27, 2026
Five years of discovery: The Wu Tsai Human Performance Alliance marks a milestone
January 26, 2026
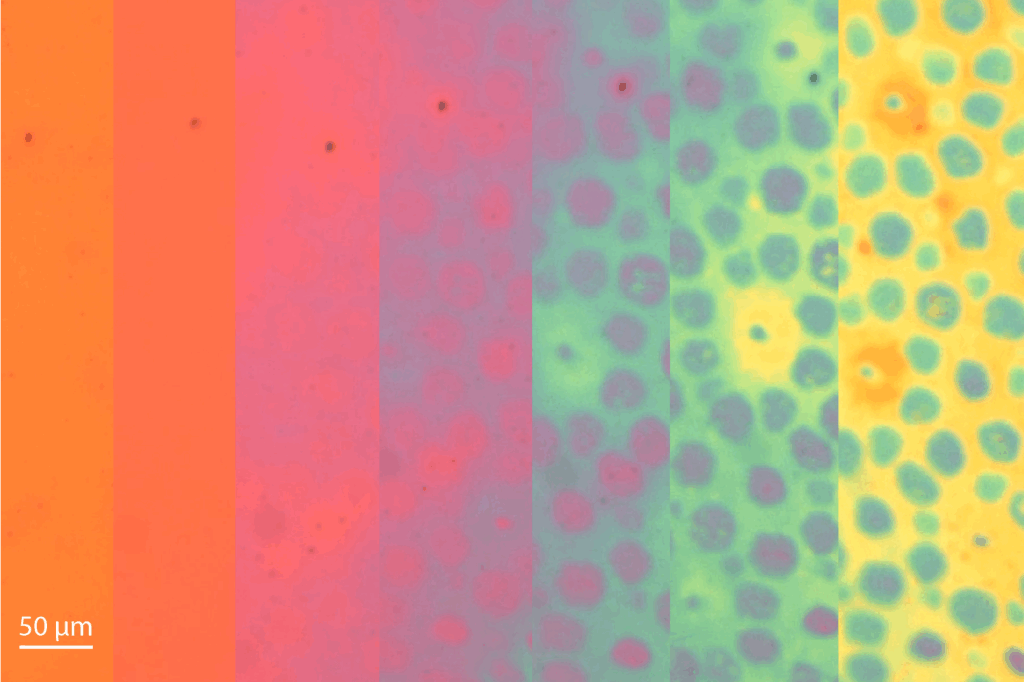
New nanoscale material that shifts color and texture may one day monitor performance signals
Get Engaged
We invite faculty, students, staff, alumni, friends, and external organizations to participate in the Wu Tsai Human Performance Alliance at Stanford.
